As of today, the cumulative number of confirmed COVID-19 cases in South Africa is 138 134 with 6 337 new cases identified.
Case Data
| Province | Total cases for 28 June 2020 | Percentage total |
| Eastern Cape | 25 099 | 18,2 |
| Free State | 1 279 | 0,9 |
| Gauteng | 36 895 | 26,0 |
| KwaZulu-Natal | 8 433 | 5,9 |
| Limpopo | 935 | 0,7 |
| Mpumalanga | 1016 | 0,7 |
| North West | 3 647 | 2,6 |
| Northern Cape | 385 | 0,3 |
| Western Cape | 60 445 | 45,0 |
| Unknown | 0 | 0,0 |
| Total | 138 134 | 100,0 |
Testing Data
A total of 1 567 084 tests have been processed cumulatively of which 38 075 tests have been conducted since the last report.
| Sector | Total tested | New tested | ||
| Private | 804 248 | 51% | 27 401 | 72% |
| Public | 762 836 | 49% | 10 674 | 28% |
| Grand Total | 1 529 009 | 38 075 |
Reported COVID-19 Deaths:
Regrettably, we report 43 more COVID-19 related deaths: This brings the total national deaths to 2 456.
We extend our condolences to the loved ones of the departed and thank the health care workers who treated the deceased.
The recoveries to date are 68 925
The provincial breakdown is as follows:
| Province | Deaths | Recoveries |
| Eastern Cape | 384 | 12 567 |
| Free State | 9 | 356 |
| Gauteng | 174 | 8580 |
| KwaZulu Natal | 109 | 3417 |
| Limpopo | 5 | 413 |
| Mpumalanga | 2 | 337 |
| North West | 5 | 433 |
| Northern Cape | 1 | 186 |
| Western Cape | 1764 | 42 636 |
| Total | 2 456 | 68 924 |
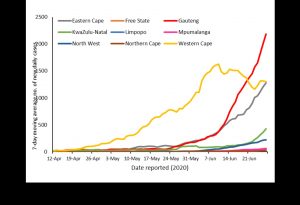
We are seeing a rapid rise in the cumulative number of positive COVID-19 cases indicating that, as we had expected, we are approaching a surge during the latter winter months of July and August.
It is anticipated that while every province will, unfortunately, witness an increase in their numbers, areas, where there is a high economic activity, will experience an exponential rise – beginning with Gauteng and Western Cape and followed by Eastern Cape and KwaZulu-Natal.
Key Provincial Issues
We believe that within the coming days, Gauteng will emerge with the highest COVID-19 numbers. Factors contributing to this trend are inward migration; the large population (especially in metros like Johannesburg, Ekurhuleni and Tshwane); increased congregating which spurs cluster outbreaks; and the level to which people are able to adapt to new behaviours such as social distancing and the wearing of masks.
When the national lockdown was eased to level three, there was a large inward movement of people as economic activities resumed. The surge that has been witnessed in the past two weeks has developed due to seeding of infections carried in by members of the community as they moved back into the workplace. It was therefore inevitable that there would be cluster outbreaks as infections spilt over from communities into places of congregation such as mines, factories, taxis and busses. (We have indeed witnessed this in the mining sector in the North West where cluster outbreaks in the mines have driven a sudden increase in the numbers in this province.)
It, therefore, remains critical to have well-established screening programmes in place at all junctures where people transition into high-density areas like in the mining sector, where we have observed quite a number of cluster outbreaks as miners return to work.
We have been engaging the Gauteng MEC for Health as well as the Provincial Department to ramp up their capacity expeditiously. In the next few days, the testing backlog will be cleared and the numbers we see will be based on a much shorter turnaround time. We have identified the need to increase COVID-19 hospital beds in this province and we will be supporting the province to ensure that they are capacitated to meet the rising demands.
In addition to regular hand washing, social distancing and the correct wearing of masks at all times, early case detection, contact tracing, quarantine and isolation are the key armaments we have in our toolbox to break the cycle of infection. The province is being engaged to strengthen their contact tracing and quarantine/isolation uptake.
The graph below clearly shows Gauteng’s steep upward curve denoting the largest surge in the country at present.
Turning our attention to the Western Cape, we recognized that there were some key issues that led the province to have a high number of cases. One of the main observations was that the provincial strategy was mainly hospicentric- focusing on case management. Intensive contact tracing, quarantine and isolation programmes were suboptimal.
Since the intervention, the province has been working hard to address these gaps but we are receiving reports that most community members remain reluctant to subject themselves to quarantine and isolation, despite the government having secured these sites in various parts of the province. Our concern is that this continues to exacerbate the risk of spread of infections in communities especially in households where it is practically impossible to self isolate given the limited space.
Although there may be provisions for authorities to enforce the law, it is important for members of the public to partner with the government in its efforts. We remain committed to working together with civil society in an empowerment exercise that enables each individual to make the right decisions – decisions that allow people to protect themselves, protect the elderly, protect those with co-morbidities and protect the poor and vulnerable. We are working on a programme with social scientists and a new multi-sectoral Ministerial Advisory Committee on Social Behavioural Change to attain fundamental reform at grassroots levels for the sake of saving lives. It will be important to engage the community, religious and traditional leaders who can motivate individuals to adhere to non-pharmaceutical interventions.
Having compared the real numbers with those depicted in predictive models, we have noticed that Western Cape hasn’t quite reached the surge as expected by modellers. The consortium has accordingly reviewed their models, taking into account what has been observed in actual terms. Since we have cleared the testing backlog, the numbers attributable to those backlogged samples no longer play a role and so the increase in new cases is reduced. Having said that, the rise is still significant and Western Cape remains a key hotspot in the country. We will, therefore, continue to support the province and pay close attention to key developments. Having discussed Western Cape, we now move to issues pertaining to its neighbour, the Eastern Cape.
I have previously spoken to the province’s vulnerability due to its proximity with Western Cape – indeed this has manifested in the trends we are seeing currently. Interprovincial migration is complicated by the fact that seasonal workers often move back and forth between both provinces. As in other provinces, carriers of the Coronavirus seed infection into spaces where people congregate and so we have also seen a number of cluster outbreaks in Eastern Cape.
Case management in Eastern Cape has also come into the spotlight. We wish to reassure the public that complaints on social media regarding treatment in some of the hospitals, as well as overall public health issues described in the media, have been well noted.
We, therefore, need to emphasize the strengthening of the provincial health system in its entirety. We had initially deployed a team of epidemiologists from the National Department of Health who intervened on an emergency basis to focus on the bottleneck in Personal Protective Equipment (PPE) procurement and the immediate outbreak response.
We are now reinforcing this support by deploying experienced senior managers to deal with the overall health systems management in the province and assist with the ground response. Once again, it will be important to carry out strong tracking and tracing systems and optimize quarantine and isolation uptakes.
Key National Issues
Understandably, there has been a lot of concern about the schooling system and the ability to successfully sustain the reopening of schools. Once again, we wish to highlight that the cluster outbreaks we are seeing in schools are a result of learners or educators who had unknowingly acquired COVID-19 in their respective communities before returning to school. It was for this reason that an intense screening and testing programme was instituted in schools to ensure the early identification of cases before they become super-spreader events. As the Department of Health, we are equally keen to ensure minimal disruption to the school calendar going forward and so we, in collaboration with our experts, are working closely with the Department of Education to strengthen protocols so that schools do not close unnecessarily because of identified cases.
Overall, we expect that all provinces will start experiencing an increase in the number of COVID-19 cases – even those with low numbers now. We are closely monitoring all districts, whether they are high-transmission or low-transmission areas. Indeed, the differentiated approach emphasized the need to increase monitoring and surveillance in low-transmission areas.
Hotpots need reinforcements and health intervention teams will be deployed for additional capacity so that the outbreak response matches the rise in numbers. The lockdown, and restrictions on large gatherings, have put in a better position to respond to the outbreak now as compared to the situation we could have been in had we allowed the virus to continue spreading unabated back in March.
Recognizing that the numbers will soon outpace manual tracking and tracing, we have piloted a tracking and tracing ICT application solution which has already demonstrated excellent efficacy in the geo-location of cases, tracking and notifying contacts, and providing information and alerts. These are proving to be wonderful communication tools, enabling us to send messages to affected individuals on their mobile phones. This tool bolsters the work of exist- ing contact tracers, whose value in engaging community members cannot be diminished by technology.
Overall, case management is very good and I would like to congratulate all officials and health care workers for tirelessly soldiering on under the most trying circumstances. We will be clearing all testing backlogs and reducing the turnaround time to less than 72 hours so that the management of persons under investigation and contacts can be expedited.
Our hospitalization rate is increasing with Western Cape remaining the province with the highest numbers of admissions. As at 27 June the majority of hospitalized patients were admitted in Western cape at 36% (1629), Gauteng at 26% (1 164) and Eastern Cape at 17% (775)
Nationally the highest proportion of patients are in general wards (isolation wards) at 80,1% of hospitalized patients, 11.3 are in intensive care and of those 58,6% are on ventilation. 15% of all hospitalized patients are on oxygen. As such, we recognize that we have not reached our full bed capacity and this is an area receiving urgent attention together with the provincial departments. Successful public and private partnerships are paramount so we are very pleased that negotiations with the private sector are now concluded and private facilities are ready to accept public patients.
We have engaged industries to secure what we need to meet our increasing oxygen requirements and we are very gratified by the cooperation and willingness of industries to divert oxygen to hospital facilities. The procurement and acquisition of ventilators is on course – we feel confident we will be able to meet demand.
We have revised the dexamethasone protocols to ensure early administration to the most critically ill patients. A further study of hospitalization data gives us insight into the natural history of the disease – this is key as we craft the national COVID-19 response.
The National Institute of Communicable Diseases has published data studying 10 700 COVID-19 admissions in 269 facilities (71 Public and 198 private) between 5 March 2020 and 21 June 2020.
The data does indeed confirm that the elderly and those with co-morbidities – like hypertension, diabetes, cardiac disease, chronic kidney disease, malignancy, HIV and obesity – are the most vulnerable population. As we are all well aware, these diseases are prevalent in our country. We, therefore, cannot afford to take our eyes off the non-COVID-19 issues that were already putting pressure on our health care system before the advent of COVID-19.
We will be using the opportunities afforded by the COVID-19 pandemic response to strengthen primary health care. We believe that investment in primary health care will ultimately have a financial benefit because healthy people build economies.
We also appeal to all citizens living with these conditions not to neglect their appointments and medication for fear of going to a facility and contracting COVID-19. We have ensured that all facilities have a triaging mechanism in place to separate those with flu-like symptoms. It is vital that everyone living with these co-morbidities ensures good control of their chronic conditions. We have also said that for those who are well controlled, clinicians are encouraged to prolong their repeat scripts for the duration of the State of Disaster. This will greatly assist in reducing facility burden and avoiding exposure for those with co-morbidities.
Although we see mortally rising in absolute numbers, our mortality rate remains stable between 1,8% and 2,1%. We can still improve this mortality rate by isolating and quarantining appropriately where required. This directly reduces exposure and protects those who are vulnerable.
Appeal to South African Citizens to Support the Campaign for Social Behavioural Change
As Government, we have mobilized every resource, every faculty and wherewithal at our disposal to effect the necessary interventions. But the government cannot manage this unilaterally. Every single South African now needs to focus on adhering to recommendations pertaining to non-pharmaceutical interventions. We are extremely concerned that fatigue seems to have set in and South Africans are letting down their guard at a time when the spread of infection is surging.
We see poor or no social distancing in communities. Masks are being abandoned or not worn properly and there is laxity setting in around frequent hand-washing. This will directly influence the rise in numbers in the next two weeks. We must all appreciate that there is a direct causal link between the surge of cases and our ability, or inability, to adhere to these very basic principles.
We do not have a vaccine. We do not have a cure. Our ability to break the cycle of infection depends on our willingness to remain focused and disciplined and take non-pharmaceutical interventions seriously.
We can beat this pandemic together – we already proved this during the lockdown. It remains in each and every citizen’s hands to admonish family members, colleagues, friends. who refuse to adhere to measures that protect lives by limiting the spread of this virus.


