
The world is increasingly facing the threat of emerging and re-emerging infectious diseases (EID) with viral RNA zoonotic pathogens playing a leading role. Biological, socio-economic, ecological and anthropogenic factors are creating conducive conditions for a storm of EIDs. Emerging zoonoses highlight the dangers of the ability of pathogens to constantly adapt, survive and infect populations of animals and people and then rapidly move between these host populations. The most recent epidemics of Ebola virus disease, Zika virus disease, and the ongoing pandemic of covid-19 demonstrate the global significance of EIDs and clearly demonstrate the lack of adequate capacities in their prevention, detection, diagnosis, surveillance, response and research. Epidemic-prone zoonoses are also a sobering reminder of the tremendous socio-economic, humanitarian and trade damage that this group of diseases can cause.
Of 1415 known pathogens of humans, 62% have an animal origin. Over the last several decades, there has been an average of almost one new emerging disease each year, and approximately 75% of these diseases have been zoonotic. Changes in our weather, climate, ecosystem, animal production systems, human behavior, economic development and land use, continue to alter the dynamic between hosts, vectors, and microbes in novel ways. Microbes continue to evolve and adapt, and now, with the tremendous acceleration and expansion of global trade, human movement and travel and the escalating population of both people and animals, the microbes have an even greater opportunity to adapt, change, and be transported to new hosts and ecosystems, often with disastrous results as exemplified by the covid-19 pandemic. Capturing and processing of wildlife for consumption and the use of their products as derivatives in traditional medicine contributes to spillover of dangerous pathogens to humans, with potential catastrophic health and socio-economic consequences. Understanding of basic virology, epidemiology and ecology of the causative agents,,is essential for the development of new generation accurate and safe point of care diagnostics,effective and safe therapeutics, and vaccines – all of which contribute to effective disease prevention and control.
The Centre for Emerging Zoonotic and Parasitic Diseases (CEZPD) of NICD-NHLS, led by Prof Janusz T. Paweska, provides national and regional capacity for the diagnosis, surveillance, and research of viral, bacterial and parasitic pathogens of public health importance, particularly those classified as zoonotic biosafety level 3 (BSL3) and biosafety level 4 (BSL4) agents. This is possible as the Special Viral Pathogens (SVP) Division of the CEZPD houses the most advanced integrated high (BSL3) and maximum (BSL4) biocontainment laboratory infrastructure in the country and on the African continent. These facilities constitute both national and regional strategic laboratory infrastructure for preparedness and response to the emergence and re-emergence of dangerous, high-consequence pathogens and bioterrorism, including highly lethal viral haemorrhagic fevers such Ebola and Marburg viral diseases, Lassa fever, Crimean Congo haemorrhagic fever and yellow fever.
Consequently, the SVP CEZPD plays a key role in the investigation of highly dangerous viral pathogens emerging from a zoonotic source, and for which no vaccines and treatments are available to date. The facility is intensively utilized for processing, storage, and characterization of the deadliest viruses known to science, their surveillance, ecology and epidemiology, the production of immunoreagents, development and validation of diagnostic tools, and for experimental studies in animals, including bats. In 2008, Prof Paweska and his team led the discovery of a new arenavirus (Lujo virus) following a fatal nosocomial outbreak in Johannesburg. In 2014-2016 he led the operation of the South African mobile molecular Ebola diagnostic laboratory in Sierra Leone as a part of international response to the unprecedented outbreak of Ebola virus disease in West Africa. This initiative represents to date the largest NICD-NHLS and SA outbreak response on foreign soil. He is a member of the African Scientific, Research and Innovation Council Technical Advisory Board on Science, Technology and Innovations for Strategic Intervention for COVID-19.
The challenges posed by the coronavirus disease 2019 (covid-19) pandemic are shaping the course of human history and there is every indication that this disease will become endemic and will continue to be significant challenge for humans in years to come. While the virus is spreading and devastating populations worldwide, it is simultaneously transforming public health, economics and politics. It has already affected 500 million people worldwide and new cases are still steeply rising in South Africa. This prompts us to mobilize all local research capacity to effectively respond to this newly emerged disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), probably of animal origin (bats?).
In the last few months NICD-NHLS scientists and biocontainment engineering and technical staff successfully commissioned safe and secure operation of a new BSL3 facility at SVP CEZPD, which is now intensively used primarily for work with SARS-CoV-2. There are a number of covid-19 diagnostic and research activities which are only allowed to be conducted under BSL3 conditions and procedures, including attempted isolation of the virus from clinical specimens, replication of the virus in cell cultures and/or laboratory animals, performing diagnostic tests requiring the use of live virus, and experimental inoculation studies. It should be emphasized here, that laboratory capacities to isolate, handle, culture and store SARS-CoV-2, constitute valuable bio-defence assets, but are also a potential biothreat to people, animals and the environment. For these reasons, it is essential that national and international regulations and practices concerning the operation of high-biocontainment facilities are implemented, executed, observed and strictly monitored to prevent the leak of the virus from these laboratories or intentional misuse. Under SA regulations, all BSL3 facilities need to be registered with the the South African Council for the Non-Proliferation of Weapons of Mass Destruction.
The NICD isolation and culturing capacity of SARS-CoV-2 from covid-19 patients, developed in last few weeks, will greatly contribute to enhancing the South African capacity in the development of diagnostics, vaccines, molecular epidemiology, and clinico-pathological studies.
Prof Paweska and his team in collaboration with the Center for Respiratory Diseases and Meningitis, NICD-NHLS, led by Prof Cheryl Cohen and Prof Anne van Gottberg, are developing in vitro microneutralization assay for the detection of neutralizing antibodies in sera from covid-19 patients. This assay is regarded as the gold standard for measuring humoral responses to infections with viruses, but also requires the use of well standardized preparations of live virus. Successful establishment of this laboratory diagnostic standard will contribute to studies on the kinetics of immune responses, including their protective role against SARS-CoV-2 infection, assist in the evaluation of covid-19 vaccines, and in pathogenesis studies. It will also aid the development of other much needed validated and accurate serological assays, e.g. ELISA and point of care lateral flow antibody detection platforms, which could be used subsequently on a massive scale outside biocontainment facilities, including primary care facilities, in epidemiological investigations aiming at monitoring the spread and transmission trends in the general population and selected high risk groups (e.g. health care workers, people with underlying conditions), and in different socio-economic settings.
The successful control of the covid-19 pandemic, and protection of people against SARS-CoV-2 infection, require a quantum leap in the development of covid-19 vaccine candidates. The current covid-19 vaccine research and development (R&D) landscape includes more than 115 vaccine candidates, being developed and subjected to different levels of pre-clinical and clinical evaluation, mostly in North America, Asia, Australia and Europe. Traditionally it takes on average over 10 years to develop and license a safe and efficacious vaccine for large-scale manufacturing and public use. It appears, however, that the scale and speed of the global vaccine R&D effort in response to the covid-19 pandemic, might deliver a vaccine by early 2021, which could be used under emergency regulations.
To consider the potential local development and manufacturing of inactivated or live-attenuated covid-19 vaccines, Prof Paweska and his team undertook characterization of replication kinetics patterns of selected local isolates of SARS-CoV-2 in different cell culture systems. One of the prerequisites to consider in the development of an inactivated vaccine, is the capacity to produce high concentrations of the virus. Generation of viral replication curves using data from in vitro experiments is one of the steps in the development of a standardized protocol for large-scale production of required viral yields.

Figure 1. Tissue culture flask with green monkey kidney cells used to isolate SARS-CoV-2 from covid-19 patients.

Figure 2. Dr Jacqueline Weyer and Prof Janusz Paweska (BSL3, SVP CEZPD NICD-NHLS) monitoring SARS-CoV-2 growth in cell culture by microscopic observation of cytopathic effects caused by a replicating virus.
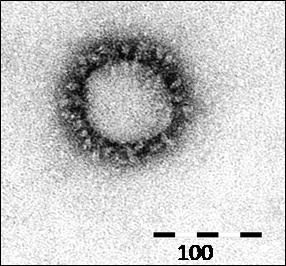
Figure 3. Eye to eye with an invisible enemy through electron microscope lenses. Virus particle of SARS-CoV-2 with a‘crown’ of peplomers, characteristic for the Coronavirus genu.s. Cultured isolate (SVPL 97/20) from a South African covid-19 patient (Electron microscope photo: Dr Monica Birkhead, SVP CEZPD).

Figure 4. Reading of SARS-CoV-2 titration results in a cell culture.